The Effect of Age on Lumbar Range of Motion a Systematic Review
Open admission peer-reviewed chapter
Pelvic Movement in Crumbling Individuals and Stroke Patients
Submitted: October 13th, 2016 Reviewed: Jan 17th, 2017 Published: May 31st, 2017
DOI: 10.5772/67510
IntechOpen Downloads
one,396
Total Affiliate Downloads on intechopen.com
Abstract
The mobility of the lumbar spine (anteversion and retroversion) may be reflected in seated pelvic mobility. When sitting with the soles of the feet in contact with the floor, friction may restrict the flexion of the knees and, consequently, the pelvic anteversion. In full general, joint mobility declines with advancing age. Lumbar spine mobility in anteversion and retroversion also decreases with advancing age. The kickoff half of this chapter is based on a report that investigated the relationship between age and the maximum pelvic anteversion and the retroversion angles in healthy volunteers. The measurements were performed with the bailiwick in a sitting position with free knee movement. On the other paw, the sit-to-stand up movement is one of the well-nigh mechanically enervating tasks undertaken during daily activity. The sacral sitting posture, which is a characteristic posture of stroke patients, is not ideal for smoothly executing the sit-to-stand up movement. Stroke patients may adopt this posture due to the need to increase sitting stability. The second one-half of this chapter discusses a study that investigated the human relationship between the pelvic anteversion and retroversion angles and the ability of stroke patients to perform the sit-to-stand up move.
Keywords
- pelvic movement
- anteversion
- retroversion
- aging
- stroke
- sit-to-stand up
*Address all correspondence to: asai@mhs.mp.kanazawa-u.ac.jp
ane. Introduction
Maintaining sagittal residual is important to both sitting and continuing. Sagittal balance, or "neutral upright sagittal spinal alignment," is a postural goal of surgical, ergonomic, and physiotherapeutic intervention [ane]. Kyphotic curvature of the spine negatively impacts the quality of life (QOL) in elderly people [ii]. Kasukawa et al. reported that the sagittal residuum was well maintained in subjects who had both a good thoracic range of motion (ROM) and good lumbar ROM and back muscle strength, which indicates that these factors are too related in maintaining sagittal residual [2]. The description of the relationship between the QOL and abnormal posture in elderly individuals may help to improve the QOL through preventive methods and exercises [three]. Although the degree of lumbar lordosis when sitting has been shown to exist weakly associated with historic period, lumbar lordosis was not found to exist affected past lifestyle, the level of physical activeness, or an private'southward type of piece of work [4]. Little is known almost the sitting posture of elderly individuals in comparison with young individuals [5]; thus, investigating the effects of aging on the sagittal spinal and pelvic alignment in the sitting position is important for clarifying the relationship betwixt pelvic motion and the QOL. Sitting positions are more often than not categorized into two types: the quiet sitting position and the functional sitting position. A person sits in the functional sitting position during (or when anticipating) physical activity. The functional sitting position therefore requires control in diverse sitting postures.
Multiple movements of the spine and pelvis are needed to maintain the various sitting positions. The human relationship between the movements of the lumbar spine and pelvis has been investigated [5, 6]. The relationship between the pelvic inclination angle and lumbar spine lordosis was more distinct in the sitting position than in the standing position [5, seven]. Thus, lumbar spine mobility (kyphosis and lordosis) may be reflected in seated pelvic mobility. However, it has been reported that joint mobility is generally reduced by aging. The trunk mobility of elderly individuals is junior to that of young people [eight–10]. In particular, lumbar spine mobility in both lordosis and kyphosis decreases with aging [1, 11, 12]. In add-on, Keorochana et al. suggested that the degeneration of the interspinous ligaments with aging is 1 of the factors that contributes to the low mobility of the lumbar spine [13]. Hence, the movement patterns of elderly individuals may be restricted when they are seated because in that location is less variety in their sitting positions in comparison with immature subjects.
The pelvic tilt in the sagittal plane may be affected by flexion and the extension mobility of the hip joints, because the pelvis moves forrard and astern effectually the hip articulation as a pivotal axis in the seated position. Since the hamstring muscles originate at the ischial tuberosity of the pelvis, the tension in the hamstring muscles has an effect on the pelvic inclination bending in the sitting position [14, 15]. Thus, a frontwards pelvic tilt may increase the tension in the hamstring muscles when sitting with a fixed knee angle and the sole of the foot in contact with the floor. Connective tissue compliance is considered a major factor in musculoskeletal flexibility [16]. Muyor et al. [17] reported that the forward pelvic tilt angle increased later on hamstring musculus stretching, and Feland et al. [16] confirmed that pelvic mobility in the sagittal aeroplane increased in elderly people after hamstring musculus stretching. The increment in the tension in the hamstring muscles when sitting with the soles of the anxiety in contact with the floor may restrict the pelvic forwards tilt. Thus, the complimentary movement of the knees should be possible during pelvic motility when sagittal plane pelvic mobility is investigated with a subject in a sitting position. However, some sitting pelvic mobility studies accept not conspicuously described human foot contact with the flooring or the knee articulation positioning [6, 18].
On the other hand, the recovery of sitting balance is ordinarily assumed to be essential for obtaining independence in other vital functions such as reaching, sit-to-stand, and sitting downwards [xix–21]. The early assessment and management of trunk control should be emphasized after stroke [22]. Many researchers have suggested that the trunk command or sitting residual of early on phase stroke patients tin predict a belatedly stage activities of daily living (ADL) result [19, 22, 23]. The sit-to-stand up job is frequently performed and this ability is considered a prerequisite for upright mobility and therefore, for performing other important daily activities such every bit locomotion [24, 25]. Riley et al. suggested that the sit-to-stand up motility is the most mechanically enervating job undertaken during daily activity [26]. The sit-to-stand movement represents a common functional movement that is practiced in the early stage of rehabilitation [27].
Stroke patients have less stability in the sitting position in comparison with age-matched healthy subjects [28–30]. The reason for this is explained in a number of reports. In stroke patients, the activity of the rectus abdominis and latissimus dorsi muscles on the afflicted side of the body is reduced and delayed in comparison to both the unaffected side and command subjects [31]. Moreover, the temporal synchronization between the pertinent muscular pairs in stroke patients is lower in comparison to good for you subjects [32]. The following factors tin as well be considered to exist related to the sitting position: firstly, stroke patients cannot adequately flex the hip when the trunk extensor muscles are contracted; secondly, it is difficult to maintain the trunk in a vertical position when the subject is seated due to the insufficiency of the abdominal muscles [33]. Thus, when stroke patients attempt to perform the sit-to-stand movement with a retroverted pelvis and kyphotic trunk, the standing up action is affected due to the insufficiency of pelvic anteversion and torso extension. In improver, Campbell et al. suggested that deficits in the muscle strength and trunk aamplitude of stroke patients result in reduced pelvic mobility, apparently equally a strategy to protect against a potential risk of loss of balance when reaching in the sitting position [34].
Numerous studies investigating torso move accept considered the supine position as 1 segment, ignoring the complexity of intervertebral movement [35]. Campbell et al. indicated that little attention has been paid to how elderly persons coordinate the head, pelvis, and trunk during motility [34]. Studies on the sitting posture of stroke patients accept a similar trend. Few studies have investigated the motion of the spine and pelvis separately. Verheyden et al. reported on pelvic movement during lateral reach movements in the sitting position [36], and Messier et al. described the movements of the upper trunk and pelvis when subjects touched a target placed in front of them with the forehead [37]. To execute the sit-to-stand up movement smoothly, the pelvis must be leaned forwards to flex the hip joint, and the trunk must be flexed in order to: (one) utilize the hip extension moment; (2) reduce the genu extension moment; and (iii) project the center of gravity within the base of support [38–43].
Pelvic mobility plays an important role in the sit-to-stand movement in elderly people and stroke patients.
This affiliate kickoff discusses the age-related changes in the maximum anteversion and retroversion of the pelvic angles in the sitting position [44] and and then explores the human relationship between the ability to perform the sit-to-stand up movement and the maximum pelvic anteversion and retroversion angles in stroke patients [45].
Advertisement
2. The age-related changes in the pelvic angles during sitting
The outset section investigated the human relationship between age and the maximum pelvic anteversion and retroversion angles, as well every bit the associated pelvic range of motion, which is measured based on the knee joint movement in the sitting position [44]. The pelvic range of move was defined as the deviation betwixt the maximum pelvic anteversion and retroversion angles. The hypothesis of the present study was that pelvic range of motion would be affected by aging.
The participants included 132 healthy volunteers (female,
| Age group | | Maximum pelvic anteversion angle (˚) | Maximum pelvic retroversion angle (˚) | Pelvic range of motion (˚) |
|---|---|---|---|---|
| twenty–29 years | | 84.5±three.4 | 123.i ± six.1 | 38.vii ± 6.0 |
| thirty–39 years | | 87.viii±four.1 | 125.7 ± 6.8 | 37.6 ± 9.2 |
| 40–49 years | | ninety.1±5.4a | 124.1 ± 8.9 | 34.0 ± viii.vii |
| 50–59 years | | 88.8±4.6a | 118.two ± 9.8 | 29.4 ± viii.4a,b |
| threescore–69 years | | 92.6±6.5a,b | 117.1 ± 8.7b | 24.3 ± 6.3a,b,c |
| 70–79 years | | nine.39 ± 4.0a,b,d | 117.8 ± nine.3 | 23.8 ± 8.6a,b,c |
Table ane.
The mean and standard departure of the pelvic angles in each age grouping [44].
Meaning difference from 20 to 29 years of age.
Significant difference from 30 to 39 years of historic period.
Significant difference from 40 to 49 years of historic period.
Significant difference from 50 to 59 years of historic period.
All measurements were taken with the participants seated on a chair with a l cm × 50 cm seat face. The tiptop of the seat face was 65 cm from the floor to allow the free motility of the genu joints. The participants sabbatum on the chair. The forepart edge of the seating face up was aligned with the point 66% forth the length of the thigh from the greater trochanter.
The pelvic angles were measured based on the sacral inclination angle [46]. An inclinometer with a resolution of 1° was used to mensurate the pelvic angles. The pelvic tilt angle was defined as the angle between the longitudinal centrality through the midline of the dorsal sacral surface and the inductive horizontal line (Figure i).

Effigy 1.
A schematic analogy of the procedure for measuring the pelvic inclination angle: (A) the pelvic retroversion angle, (B) the pelvic anteversion bending [
The subjects were instructed to maintain the same anteroposterior shoulder position throughout the movements of pelvic inclination to avoid anteroposterior motility of the body. The instruction to the subjects was, "Please maintain your shoulder position during pelvic movement." Participants assumed alternating maximum pelvic anteversion and retroversion positions v times. The maximum and minimum angles were excluded, and the hateful of the three remaining values was calculated. The pelvic range of motility was defined equally the difference between the average maximum pelvic anteversion and retroversion angles.
The maximum pelvic anteversion bending, maximum pelvic retroversion angle, and the range of pelvic movement were significantly afflicted by aging (Table 1).
The maximum pelvic anteversion angles in participants of forty–49, 50–59, threescore–69, and lxx–79 years of historic period were significantly smaller than those in participants of 20–29 years of historic period. The maximum pelvic anteversion angles in participants of 60–69 and 70–79 years of age were significantly smaller than those in participants of xxx–39 years of age, and the maximum pelvic anteversion angles in participants of 70–79 years of age were significantly smaller than those in participants of 50–59 years of age (Tabular array 1).
With regard to the maximum pelvic retroversion bending, none of the age groups showed a pregnant deviation in comparison to the 20–29 year age group. The maximum pelvic retroversion angle in the participants of 60–69 years of historic period was significantly smaller than that in the participants of 30–39 years of historic period (Table 1).
The pelvic ranges of move in participants of fifty–59, 60–69, and 70–79 years of age were significantly smaller in comparing to participants of 20–29 and 30–39 years of age. Furthermore, the pelvic range of motion of participants of 60–69 and 70–79 years of historic period was significantly smaller than that in participants of 40–49 years of historic period (Table one).
The relationships betwixt these variables and historic period were approximated using linear regression equations (Figure two). These results indicate that pelvic mobility in the sitting position is affected by aging. In that location was a significant correlation between age and the maximum pelvic anteversion bending (

Figure 2.
The correlations between age and the maximum pelvic anteversion bending (black circles), the maximum pelvic retroversion bending (white squares), and the pelvic range of motion (black triangles) [
Hamstring tension probably had an insignificant effect on pelvic mobility in this dataset, especially on the anterior tilt, because the knees could movement freely during pelvic motion. The hip flexion angle during maximum pelvic anteversion was 87° and the extension angle during maximum retroversion was 57° in participants of 70–79 years of historic period. Thus, the pelvic mobility in the present study did non seem to be afflicted by hamstring muscle tension or hip joint mobility. The pelvic mobility measured in this study was in line with the results of previous studies on lumbar spine mobility, which reported strong correlations betwixt pelvic tilt or the sacral tilt angle, and the lumbar spine lordosis bending in the sitting position [5, 46, 47]. In addition, the pelvic mobility in the sitting position is larger than that in the standing position [6]. Kuo et al. reported that at that place was a significant correlation betwixt lumbar spine mobility and the pelvic tilt angle (
However, due to the aging-related shortening of the hamstring muscles, the maximum pelvic anteversion angle may be more restricted when performing this movement without the gratuitous mobility of the knees.
The pelvic range of movement was approximately twoscore° in participants of 20–29 years of historic period and approximately 24° in participants of lx–69 and lxx–79 years of age. The charge per unit of pelvic mobility limitation that occurred with aging in this report (approximately 30%) was larger than that previously reported for hip extension (approximately xx%), which is considered to exist the articulation in the lower extremities that is well-nigh express by aging [48]. Thus, sagittal aeroplane pelvic mobility may exist an important factor that is associated with mobility limitation during the sit-to-stand move in elderly adults.
Advertisement
3. The human relationship between the ability to perform the sit down-to-stand motility and the pelvic angles in patients with stroke
The sacral sitting posture, which involves a high degree of trunk flexion and neck extension, is frequently observed in stroke patients. This sitting posture is not the platonic posture for smoothly performing the sit-to-stand up motion. Maintaining the sitting position with pelvic retroversion may be necessary to increase the sitting stability of stroke patients. However, the ability to achieve anteversion of the pelvis is necessary to perform the sit-to-stand motion.
The second department investigates the human relationship between the pelvic anteversion and retroversion angles and the ability to perform the sit-to-stand up movement [45]. The hypothesis of this study was that stroke patients who are able to stand up from sitting in a chair have a larger maximum pelvic anteversion bending than patients who are unable to stand from a chair.
30-ii hemiparetic subjects (female person,
The participants sat on the chair, with the front edge of the seat aligned with the point corresponding to 66% of their thigh length from the greater trochanter. The subjects sat with their feet in the parallel position with both artillery crossed on their chest and with no support for the body or upper extremities. The chair seat meridian was adjusted to 100% of the subject's lower leg length (the distance from the lateral femoral condyle to the footing); the knee joint flexion angle was 90°.
The pelvic angles were measured according to the sacral inclination angle (Figure 3). Pelvic anteversion was reported as a positive angle and pelvic retroversion was reported equally a negative angle. The subjects were instructed to maintain the initial acromion anteroposterior position during the movements to avert trunk anteroposterior motion. The stroke patients (barefoot) were and so asked to stand at a cocky-selected speed while keeping the arms folded across the chest. Three trials were performed with no restrictions on the position of the feet. Stroke patients who could independently perform all 3 trials were classified into the stand-able group. The remaining patients were classified into the stand up-unable grouping.

Figure 3.
A schematic illustration of the procedure for measuring the pelvic inclination bending: (A) the pelvic retroversion angle, (B) the pelvic anteversion bending [
The maximum pelvic anteversion bending in the stand up-able, stand-unable, and command groups ranged from 5 to −4°, −5° to −22°, and 10° to −13°, respectively (Figure four). In the stand-able grouping, the maximum pelvic anteversion angles were all in a higher place −5°; in contrast, to the angles in the stand-unable grouping were all beneath −5° (Figure 4). The mean and standard deviation of the maximum pelvic anteversion angles in the stand-able, the stand-unable, and control groups were 1.2 ± 2.8°, −12.4 ± 6.1°, and −1.half dozen ± 5.0°, respectively. The group was found to have a significant main effect (
| Stand-able group ( | Stand-unable grouping ( | Command group ( | ||
|---|---|---|---|---|
| Maximum pelvic | Mean ± SD | i.2 ± 2.8 | −12.four ± 6.1a,b | −1.half-dozen ± 5.0 |
| anteversion angle (º) | Range (max–min | five to −4 | −5 to −22 | 10 to −13 |
| Maximum pelvic | Mean ± SD | −18.five ± v.6b | −19.6 ± iv.6b | −27.6 ± 8.1 |
| retroversion angle (º) | Range (max–min) | −30 to −10 | −27 to − x | −46 to −10 |
| Range of pelvic move | Mean ± SD | 19.vii ± 5.1b | seven.2 ± 5.1b | 25.9 ± 7.half dozen |
| (º) | Range (max–min) | 28 – ten | 15 – 0 | 49 – 9 |
Tabular array 2.
The hateful and standard divergence of the pelvic in the stand-able, stand-unable, and control groups [45].
Meaning departure from the stand-able group.
Meaning difference from command group.
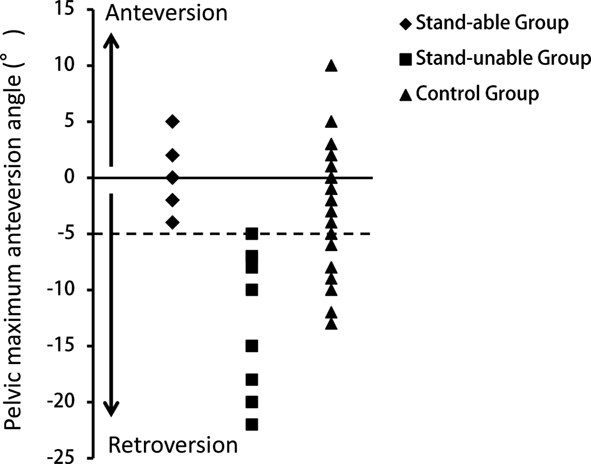
Figure iv.
The distribution of the pelvic angles in the stand-able, stand-unable, and command groups.
The maximum pelvic retroversion angles in the stand-able, stand-unable, and command groups ranged from −10° to −30°, −10° to −27°, and −10° to −46°, respectively (Table ii). The mean and standard deviation of the maximum pelvic retroversion angles in the stand-able, stand up-unable, and command groups were −eighteen.5 ± 5.6°, −19.6 ± 4.six°, and −27.vi ± 8.1°, respectively (Table two). The group was institute to accept a meaning main effect. Pregnant differences were institute between the control grouping and the stand-able group, and between the control group and the stand-unable group (Table 2). The maximum pelvic retroversion angle in the control group was significantly larger than that in both groups of stroke patients (Table two). The maximum pelvic retroversion angles of the stand-able and stand-unable groups did not differ to a statistically meaning extent (Table 2).
The range of pelvic motion in the in the stand-able, stand-unable, and control groups ranged from ten to 28°, 0 to fifteen°, and 9 to 49°, respectively (Table 2). The mean and standard deviation of the range of pelvic move in the stand-able, stand-unable, and control groups was 19.7 ± v.1°, 7.2 ± 5.ane°, and 25.9 ± 7.six°, respectively (Table 2). The range of pelvic motion in the stand-unable group was significantly smaller in comparison to the stand-able and control groups (Tabular array two).
The hypotheses that the maximum pelvic anteversion angle and the range of pelvic motion in the stand-able group would be significantly larger in comparing to the stand-unable group were confirmed. Information technology is noteworthy that there was a cutting-off value maximum pelvic anteversion bending that could divide stroke patients into the stand-able and stand-unable groups. The data propose that, in social club for stroke patients to perform the sit-to-stand movement, the maximum pelvic anteversion angle should be greater than −5°.
To smoothly execute the sit down-to-stand motion, the pelvis is anteverted to flex the hip joint and the torso to perform the hip extension moment, reduce the knee extension moment, and project the middle of gravity into the base of operations of support [38–43]. The sitting position stability of stroke patients has been shown to exist worse than that in historic period-matched healthy subjects [v, 11, 12]. It has been shown that stroke patients cannot sufficiently flex the hip joint when it is necessary to actuate the trunk extensor muscles during sitting [33]. Stroke patients usually sit with kyphosis and pelvic retroversion to avert falling backward due to insufficient function of the intestinal muscles. Thus, when performing the sit-to-stand motion, stroke patients may demand to lean the trunk further forward to shift the heart of gravity into the base of support using their feet due to the increased kyphosis and pelvic retroversion. Lecours et al. observed that, when performing the sit-to-stand motility, the body angle during frontwards leaning in stroke patients was larger than that in healthy subjects [35]. Hesse et al. reported that the average centre of gravity projection in the base of support in stroke patients was 3 cm behind that of healthy subjects during the seat off phase in the sit down-to-stand movement [49]. In addition, when the torso is flexed, the hip extension moment becomes insufficient due to the lack of pelvic anteversion; thus, stroke patients may depend primarily on the genu extension motility to stand up.
Some studies have reported a high correlation between pelvic inclination in the sitting position and the degree of lumbar lordosis [5] and a strong relationship betwixt the sacral angle of inclination and the degree of lumbar lordosis [46, 47]. Hence, pelvic inclination (anteversion and retroversion) reflects lumbar movement (lordosis and kyphosis). The range of pelvic movement in the stand-unable grouping was extremely express, reaching merely 28% of the control group and 36% of the stand-able group. Appropriately, in the stand up-unable group, the lumbar spine motion in the sagittal plane (lordosis and kyphosis) was probably limited in comparison to the control grouping and the stand up-able grouping.
The pelvic bending measurements were conducted in the sitting position while the field of study maintained 90° of knee joint flexion with their feet in contact with the ground. In the sitting position, the hip joints piece of work every bit pivotal axes in pelvic anteversion and retroversion. One factor that should influence the range of motion of the hip is the extensibility of the hamstrings, which bulldoze the hip and knee as biarticular muscles. Hamstring stretching was shown to improve the pelvic anteversion angle [17] and the mobility of the hip in elderly individuals [16]. The sitting position in this report fixed the knee flexion bending at xc°, which should have increased hamstring tension during the measurement. Thus, information technology is likely that pelvic anteversion was restrained past the increased tension of the hamstrings.
Cheng et al. reported the following three characteristics of the sit-to-stand movement of stroke fallers, the stroke nonfallers, and good for you subjects: stroke patients, specially fallers, required a significantly longer time to perform the sit down-to-stand movement; the rate of increase in vertical forcefulness (%BW/sec) in stroke fallers was significantly lower in comparison with nonfallers and good for you subjects; and the overshoot of vertical force (%BW) in stroke fallers was significantly lower than that in nonfallers and good for you subjects [l]. These characteristics of stroke fallers may exist associated with their limited pelvic anteversion during the sit-to-stand movement. Messier et al. suggested that, to execute the trunk flexion chore, stroke patients used a compensatory strategy that consisted in using mainly the upper trunk flexion because they were unable to tilt their pelvis anteriorly [37]. Thus, our data, which showed that the maximum pelvic anteversion bending of the stand-unable group was significantly smaller than that of the stand-able and control groups, were supported by these reports. Another point of view that should exist mentioned is that Prudente et al. suggested that neuromuscular coordination abnormalities occurred in both of the lower limbs of stroke patients during the sit-to-stand movement [51].
On the other hand, since there was no significant difference in the maximum pelvic retroversion bending of the ii stroke groups, information technology becomes clear that this angle does not affect the patient's ability to perform the sit down-to-stand movement. However, it was too demonstrated that the range of pelvic movement in stroke patients was markedly restricted in comparison to healthy subjects. In stroke patients, pelvic anteversion appears to be an important factor for regaining the ability to perform the sit down-to-stand movement.
Advertisement
4. Relevance to concrete therapy
This session demonstrated that the pelvic range of movement was affected by aging, especially in the anteversion angle, and that the maximum pelvic anteversion angle and the range of pelvic motion in the stand-able group were significantly larger than those in the stand up-unable group. Notably, if these patients are to exist able to perform the sit-to-stand movement, it is important that they acquire a pelvic anteversion angle of greater than −5°.
The mobility of the lumbar spine, which is associated with the strength and coordination of the trunk and the lower limbs, should be considered as the background of these results. The physical therapy program described beneath would help equally an initial step for improving the concrete part of elderly individuals and stroke patients—specially with regard to improving their sit-to-stand movement.
For elderly individuals: (one) pelvic anteversion and retroversion—the patient should maintain a seated position with their feet contacting the floor in a parallel position and motion slowly, alternating the pelvis from maximum anteversion to maximum retroversion. They should maintain the same shoulder anteroposterior position throughout the pelvic inclination movements in society to avoid anteroposterior motion of the trunk. (2) Leaning the trunk forrard with pelvic anteversion—the patient should lean their trunk frontward maintaining pelvic anteversion in a seated position with their feet contacting to the floor. This movement should be performed slowly and repeated. It is of import to perceive the increasing load to the lower limb during the leaning of the trunk.
For stroke patients: equally shortly as the stroke patient has obtained an independent sitting position, the treatment should focus on the mobility of the trunk and weight transfer to the lower limbs, using the same methods as for elderly individuals.
References
- ane.
Been E, Kalichman Fifty: Lumbar lordosis. Spine J. 2014; 14 :87–97. DOI: x.1016/j.spinee.2013. 07.464. - two.
Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Noguchi H, Kamo K, et al.: Relationships between falls, spinal curvature, spinal mobility and dorsum extensor strength in elderly people. J Bone Miner Metab. 2010; 28 :82–87. DOI: 10.1007/s00774-009-0107-i. - 3.
Imagama S, Matsuyama Y, Hasegawa Y, Sakai Y, Ito Z, Ishiguro N: Dorsum muscle strength and spinal mobility are predictors of quality of life in centre-aged and elderly males. Eur Spine J. 2011; 20 :954–961. DOI: 10.1007/s00586-010-1606-4. - four.
Nourbakhsh MR, Moussavi SJ, Salavati M: Effects of lifestyle and work-related concrete action on the degree of lumbar lordosis and chronic low dorsum hurting in a Heart E population. J Spinal Disord. 2001; 14 :283–292. - v.
Kuo YL, Tully EA, Galea MP: Video analysis of sagittal spinal posture in healthy young and older adults. J Manipulative Physiol Ther. 2009; 32 :210–215. DOI: 10.1016/j.jmpt.2009.02.002. - six.
Endo K, Suzuki H, Nishimura H, Tanaka H, Shishido T, Yamamoto K: Sagittal lumbar and pelvic alignment in the continuing and sitting positions. J Orthop Sci. 2012; 17 :682–686. DOI: 10.1007/s00776-012-0281-1. - 7.
Youdas JW, Grarrett TR, Harmsen S, Suman VJ, Carey JR: Lumbar lordosis and pelvic inclination of asymptomatic adults. Phys Ther. 1996; 76 :1066–1081. - eight.
Kienbacher T, Paul B, Habenicht R, Starek C, Wolf 1000, Kollmitzer J, et al.: Age and gender related neuromuscular changes in trunk flexion-extension. J Neuroeng Rehabil. 2015;12:iii. DOI: 10.1186/1743-0003-12-3. - 9.
Lee ES, Ko CW, Suh SW, Kumar S, Kang IK, Yang JH: The result of historic period on sagittal airplane profile of the lumbar spine according to continuing, supine, and various sitting positions. J Orthop Surg Res. 2014; 9(1):11. DOI: x.1186/1749-799X-ix-11. - 10.
Sung PS: Different coordination and flexibility of the spine and pelvis during lateral angle between young and older adults. Hum Mov Sci. 2016; 46 :229–238. DOI: 10.1016/j.humov.2016.01.001. - 11.
Intolo P, Milosavljevic S, Baxter DG, Carman AB, Pal P, Munn J: The effect of historic period on lumbar range of movement: a systematic review. Man Ther 2009; 14 : 596–604. DOI: 10.1016/j.math.2009.08.006. - 12.
Sullivan MS, Dickinson CE, Troup JD: The influence of age and gender on lumbar spine sagittal plane range of motion. A written report of 1126 good for you subjects. Spine. 1994; nineteen :682–686. - 13.
Keorochana G, Taghavi CE, Tzeng ST, Morishita Y, Yoo JH, Lee KB, et al.: Magnetic resonance imaging grading of interspinous ligament degeneration of the lumbar spine and its relation to aging, spinal degeneration, and segmental motion. J Neurosurg Spine. 2010; 13 : 494–499. DOI: 10.3171/2010.4.SPINE09515. - fourteen.
Congdon R, Bohannon R, Tiberio D: Intrinsic and imposed hamstring length influence posterior pelvic rotation during hip flexion. Clin Biomech (Bristol, Avon). 2005; 20 :947–951. - xv.
López-Miñarro PA, Muyor JM, Belmonte F, Alacid F: Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. J Hum Kinet. 2012; 31 :69–78. DOI: x.2478/v10078-012-0007-7. - 16.
Feland JB, Myrer JW, Schulthies SS, Fellingham GW, Measom GW: The effect of elapsing of stretching of the hamstring muscle group for increasing range of move in people aged 65 years or older. Phys Ther. 2001; 81 :1110–1117. - 17.
Muyor JM, López-Miñarro PA, Casimiro AJ: Issue of stretching program in an industrial workplace on hamstring flexibility and sagittal spinal posture of adult women workers: A randomized controlled trial. J Dorsum Musculoskelet Rehabil. 2012; 25 :161–169. DOI: 10.3233/BMR-2012-0323. - 18.
O'Sullivan Grand, O'Sullivan P, O'Sullivan Fifty, Dankaerts Westward: What do physiotherapists consider to be the all-time sitting spinal posture? Man Ther. 2012; 17 :432–437. DOI: 10.1016/j.math.2012.04.007. - 19.
Franchignoni FP, Tesio L, Ricupero C, Martino MT: Torso control test as an early predictor of stroke rehabilitation outcome. Stroke. 1997; 28 :1382–1385. - 20.
Pollock Equally, Durward BR, Rowe PJ, Paul JP: The effect of independent practise of motor tasks by stroke patients: A pilot randomized controlled trial. Clin Rehabil. 2002; 16 :473–480. - 21.
Tessem S, Hagstrøm Northward, Fallang B: Weight distribution in standing and sitting positions, and weight transfer during reaching tasks, in seated stroke subjects and good for you subjects. Physiother Res Int. 2007; 12 :82–94. - 22.
Hsieh CL, Sheu CF, Hsueh IP, Wang CH: Trunk control equally an early predictor of comprehensive activities of daily living office in stroke patients. Stroke. 2002; 33 :2626–2630. - 23.
Loewen SC, Anderson BA: Predictors of stroke outcome using objective measurement scales. Stroke. 1990; 21 :78–81. - 24.
Bohannon RW, Barreca SR, Shove ME, Lambert C, Masters LM, Sigouin CS: Documentation of daily sit down-to-stands performed past community-dwelling adults. Physiother Theory Pract. 2008; 24 :437–442. DOI: 10.1080/09593980802511813. - 25.
Dall PM, Kerr A: Frequency of the sit to stand up chore: An observational study of free-living adults. Appl Ergon. 2010; 41 :58–61. DOI: 10.1016/j.apergo.2009.04.005. - 26.
Riley PO, Schenkman ML, Mann RW, Hodge WA: Mechanics of a constrained chair-rise. J Biomech. 1991; 24 :77–85. - 27.
Brunt D, Greenberg B, Wankadia S, Trimble MA, Shechtman O: The effect of human foot placement on sit down to stand in healthy young subjects and patients with hemiplegia. Arch Phys Med Rehabil. 2002; 83 :924–929. - 28.
Genthon N, Vuillerme N, Monnet JP, Petit C, Rougier P: Biomechanical cess of the sitting posture maintenance in patients with stroke. Clin Biomech (Bristol, Avon). 2007; 22 :1024–1029. - 29.
Perlmutter S, Lin F, Makhsous M: Quantitative analysis of static sitting posture in chronic stroke. Gait Posture. 2010; 32 : 53–56. DOI: ten.1016/j.gaitpost.2010.03.005. - thirty.
van Nes IJ, Nienhuis B, Latour H, Geurts AC: Posturographic assessment of sitting remainder recovery in the subacute stage of stroke. Gait Posture. 2008; 28 :507–512. DOI: 10.1016/j.gaitpost.2008.03.004. - 31.
Dickstein R, Shefi S, Marcovitz E, Villa Y: Anticipatory postural adjustment in selected body muscles in post stroke hemiparetic patients. Arch Phys Med Rehabil. 2004; 85 :261–267. - 32.
Dickstein R, Shefi Southward, Marcovitz Eastward, Villa Y: Electromyographic activity of voluntarily activated trunk flexor and extensor muscles in post-stroke hemiparetic subjects. Clin Neurophysiol. 2004; 115 :790–796. - 33.
Davis PM: Issues associated with the loss of selective body action in hemiplegia. In: Right in the middle. New York: Springer-Verlag; 1990. pp. 31–65. - 34.
Campbell FM, Ashburn AM, Pickering RM, Burnett Thou: Head and pelvic movements during a dynamic reaching task in sitting: Implications for physical therapists. Arch Phys Med Rehabil. 2001; 82 :1655–1660. - 35.
Lecours J, Nadeau S, Gravel D, Teixera-Salmela L: Interactions between foot placement, trunk frontal position, weight-begetting and knee moment asymmetry at seat-off during rising from a chair in healthy controls and persons with hemiparesis. J Rehabil Med. 2008; 40 :200–207. DOI: 10.2340/16501977-0155. - 36.
Verheyden Thou, van Duijnhoven HJ, Burnett M, Littlewood J, Kunkel D, Ashburn AM: Kinematic analysis of head, torso, and pelvis motility when people early after stroke reach sideways. Neurorehabil Neural Repair. 2011; 25 : 656–663. - 37.
Messier Southward, Bourbonnais D, Desrosiers J, Roy Y: Dynamic analysis of trunk flexion later on stroke. Arch Phys Med Rehabil. 2004; 85 :1619–1624. - 38.
Fujimoto M, Chou LS: Dynamic residuum control during sit down-to-stand up movement: An test with the middle of mass acceleration. J Biomech. 2012; 45 :543–548. DOI: ten.1016/j.jbiomech.2011.11.037. - 39.
Nikfekr E, Kerr K, Attfield S, Playford DE: Trunk motion in Parkinson'south illness during ascent from seated position. Mov Disord. 2002; 17 :274–282. - 40.
Tully EA, Fotoohabadi MR, Galea MP: Sagittal spine and lower limb motility during sit down-to-stand in salubrious young subjects. Gait Posture. 2005; 22 :338–345. - 41.
Janssen WG, Bussmann HB, Stam HJ: Determinants of the sit-to-stand up movement: A review. Phys Ther. 2002; 82 :866–879. - 42.
Schenkman M, Berger RA, Riley PO, Mann RW, Hodge WA: Whole-body movements during rising to standing from sitting. Phys Ther. 1990; 70 :638–651. - 43.
Ishigaki Due north, Kimura T, Usui Y, Aoki Thousand, Narita Due north, Shimizu 1000, et al.: Effect of ageing on quadriceps muscle strength and on the forrard shift of center of force per unit area during sit down-to-stand up movement from a chair. J Phys Ther Sci. 2005; 17 :23–28. DOI: 10.1016/j.jbiomech.2011.04.016. - 44.
Asai H, Tsuchiyama H, Hatakeyama T, Inaoka PT, Murata Thou: Age-related changes in maximum pelvic anteversion and retroversion angles measured in the sitting position. J Phys Ther Sci. 2014; 26 :1959–1961. DOI: x.1589/jpts.26.1959. - 45.
Asai H, Tsuchiyama H, Hatakeyama T, Inaoka PT, Murata K: Relationship between the power to perform the sit-to-stand movement and the maximum pelvic anteversion and retroversion angles in patients with stroke. J Phys Ther Sci. 2015; 27 :985–988. DOI: 10.1589/jpts.27.985. - 46.
Kobayashi T, Atsuta Y, Matsuno T, Takeda N: A longitudinal report of coinciding sagittal spinal alignment in an adult cohort. Spine. 2004; 29 :671–676. - 47.
Amonoo-Kuofi HS: Changes in the lumbosacral angle, sacral inclination and the curvature of the lumbar spine during aging. Acta Anat. 1992; 145 :373–377. - 48.
Roach KE, Miles TP: Normal hip and knee joint agile range of motility: The relationship to age. Phys Ther. 1991; 71 :656–665. - 49.
Hesse South, Schauer M, Malezic M, Jahnke M, Mauritz KH: Quantitative analysis of rising from a chair in healthy and hemiparetic subjects. Scand J Rehabil Med. 1994; 26 :161–166. - 50.
Cheng PT, Liaw MY, Wong MK, Tang FT, Lee MY, Lin PS: The sit down-to-stand movement in stroke patients and its correlation with falling. Arch Phys Med Rehabil. 1998; 79 :1043–1046. - 51.
Prudente C, Rodrigues-de-Paula F, Faria CD: Lower limb muscle activation during the sit-to-stand job in subjects who accept had a stroke. Am J Phys Med Rehabil. 2013; 92 :666–675. DOI: 10.1097/PHM.0b013e318282c87a.
Submitted: October 13th, 2016 Reviewed: January 17th, 2017 Published: May 31st, 2017
© 2017 The Author(southward). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution three.0 License, which permits unrestricted utilize, distribution, and reproduction in any medium, provided the original work is properly cited.
Source: https://www.intechopen.com/chapters/54689
0 Response to "The Effect of Age on Lumbar Range of Motion a Systematic Review"
Post a Comment